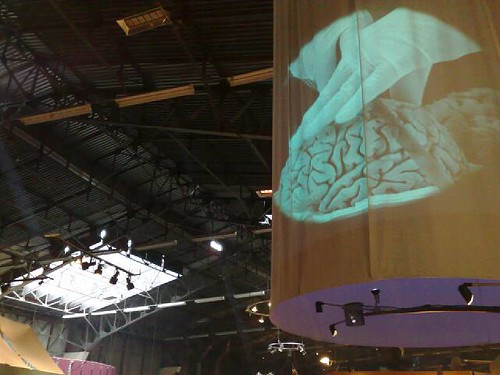
In Rest, I talk about how sleep turns out to be a form of what I call “active rest:” rest in which the body is actually doing things behind the scenes. One of the most important things it does is fire up glial cells, which you can think of as a kind of scaffolding and support system for the brain, to clear out the various toxins that build up in the brain during its normal activity. (You can think of these proteins as a kind of waste, just like the rest of the waste your body produces.)
A few years ago, neuroscientist Maiken Nedergaard observed this system at work in the brains of mice. Now, writing in Science News, Laura Bell reports on new research on human subjects indicating that “The brain may clean out Alzheimer’s plaques during sleep.” (Also, Bell’s article is a terrific overview of the history of this research, and its major lines of investigation.)
University of Wisconsin neuroscientist Barbara Bendlin has been working on the “Wisconsin Registry for Alzheimer’s Prevention, a study of more than 1,500 people who were ages 40 to 65 when they signed up” in 2001. So by now the Registry has 17 years of data, gathered from surveys, doctor’s exams, cognitive tests, even cerebral spinal fluid taps. (I love longitudinal studies like these: they reveal things that no other kind of research can.)
What Bedlin is finding is more evidence of a connection between sleep deprivation and the buildup of amyloid-beta protein fragments, which have been theorized to be one mechanism behind Alzheimer’s:
Bendlin and her colleagues identified 98 people from the registry who recorded their sleep quality and had brain scans. Those who slept badly — measured by such things as being tired during the day — tended to have more A-beta plaques visible on brain imaging….
In a different subgroup of 101 people willing to have a spinal tap, poor sleep was associated with biological markers of Alzheimer’s in the spinal fluid…. The markers included some related to A-beta plaques, as well as inflammation and the protein tau, which appears in higher levels in the brains of people with Alzheimer’s.
Now, it’s important to note that the casual arrow between poor sleep and Alzheimer’s isn’t yet clear: scientists aren’t yet willing to say with certainty whether bad sleep increases your odds of developing the disease, or whether the mechanisms that are responsible for Alzheimer’s also disrupt your sleep. As Bell puts it, Bell notes that
most studies have a chicken-and-egg problem. Alzheimer’s is known to cause difficulty sleeping. If Alzheimer’s both affects sleep and is affected by it, which comes first?
But even though “the direction and the strength of the cause-and-effect arrow remain unclear,” she continues,
approximately one-third of U.S. adults are considered sleep deprived (getting less than seven hours of sleep a night) and Alzheimer’s is expected to strike almost 14 million U.S. adults by 2050 (5.7 million have the disease today).
Either way, it’s yet another argument for taking sleep seriously, and getting enough of it.